Vision Care Misconceptions Part 3: Vision Benefits Don’t Impact Member Satisfaction
Leverage Vision Benefits to Boost Member Satisfaction
This is the third of our four-part series on Common Vision Care Misconceptions Among Health Plans. In part two, we diffused the argument that vision benefits don’t reduce medical spend. Part three breaks down the misconception that vision care doesn’t impact satisfaction, then shares ideas for leveraging vision benefits to produce healthier, happier members.
 Healthy members are happy members. And vision benefits can play a significant role in improving both.
Healthy members are happy members. And vision benefits can play a significant role in improving both.
According to the 2025 Medicare Vision Insights Report from VSP® Vision Care, vision services are highly utilized by Medicare members. Of all Medicare members surveyed in the report, 81% used their vision benefits within the past two years. Of those who had vision coverage through Medicare Advantage (MA), 94% used their annual eye exam benefit, and more than two-thirds used their prescription glasses benefit.
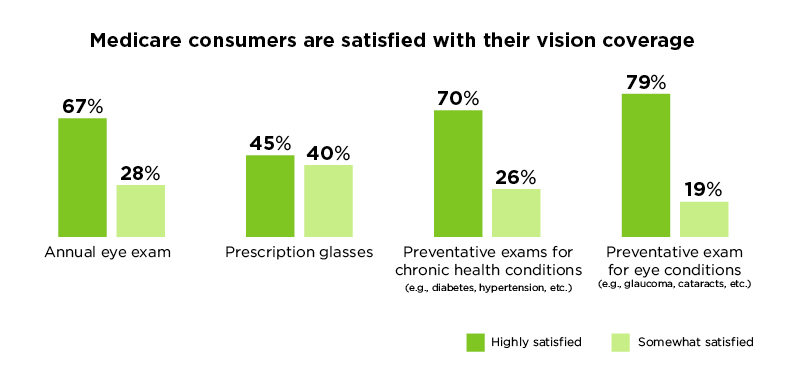
And according to the data, as utilization goes up, so does member satisfaction. For the most commonly used vision benefits, member satisfaction rates were exceptionally high:
- Preventative exams for chronic conditions benefit – 96% overall satisfaction rating
- Preventative exams for eye conditions benefit – 98% overall satisfaction rating
- Annual eye exam benefit – 95% overall satisfaction rating
- Prescription glasses benefit – 85% overall satisfaction rating
Satisfaction ratings for utilized vision benefits:
High member satisfaction requires each element of your plan contributing to a positive overall experience. It’s comforting to know with satisfaction ratings like these that vision benefits not only pull their own weight, but they can also pick up the slack if other parts of your plan aren’t performing as well.
How to Leverage Vision Benefits to Boost Medicare Plan Satisfaction
Since utilization of annual eye exams is high, providers and plans can use the exam as an opportunity to screen Medicare members for signs of chronic diseases—especially those who elect not to use annual wellness visits. They can take this opportunity to get patients in the door and potentially identify signs of chronic diseases, which leads to earlier treatment, more positive outcomes, and healthier, happier members.1
 Additionally, health plans can run campaigns to increase annual eye exam utilization rates based on the main reasons members reported missing their annual eye exam. Some of the most common include:
Additionally, health plans can run campaigns to increase annual eye exam utilization rates based on the main reasons members reported missing their annual eye exam. Some of the most common include:
- Lack of noticeable vision problems
- High out-of-pocket costs
- Forgetting to use them
- Lack of transportation
- Difficulty finding a provider
With this information in hand, you could publish an email series or video interview an optometrist explaining why a member would need an eye exam even if they didn’t notice vision problems. Explore the data and get creative with strategies for putting more members in front of their eye doctor.
Caveat! Not All Vision Benefits Are Created Equal
It’s important to keep in mind when creating campaigns based on the reasons for non-use that your vision plan needs to help overcome the obstacles that impeded members in the first place.
For example, if beneficiaries are having trouble finding a provider, you’ll need a carrier with an expansive network and a variety of care choices (i.e., private practice, retail chains, big-box retailers). A user-friendly resource for finding doctors in network is also extremely helpful.
If a high percentage of your members forget to use their benefits, look for a vision carrier that shares the load when it comes to reminding beneficiaries to schedule their annual exam.
Working together, you and your vision benefits provider can increase utilization and support better health outcomes. When you do, you’ll see member satisfaction, as well as your market share grow.
In our fourth and final installment of our series, we’ll battle the misconception that all vision coverage is the same.
Let’s Turn Insights into Action
We’re here to support you. As the only national not-for-profit vision company, VSP looks at benefits through a different lens. We're focused on maximizing vision benefits for our partners and your members. It all comes together with our single-source solution for better vision care—custom plans, improved value, and healthier members.
If you have questions or need further assistance, we’re just a conversation away.
Schedule a free consultation and learn how we can adapt these insights for your Medicare Advantage plans.
1 Centers for Medicare & Medicaid Services. (2025.) 2022 Use of Preventive Care Services Among Medicare Beneficiaries PUF.